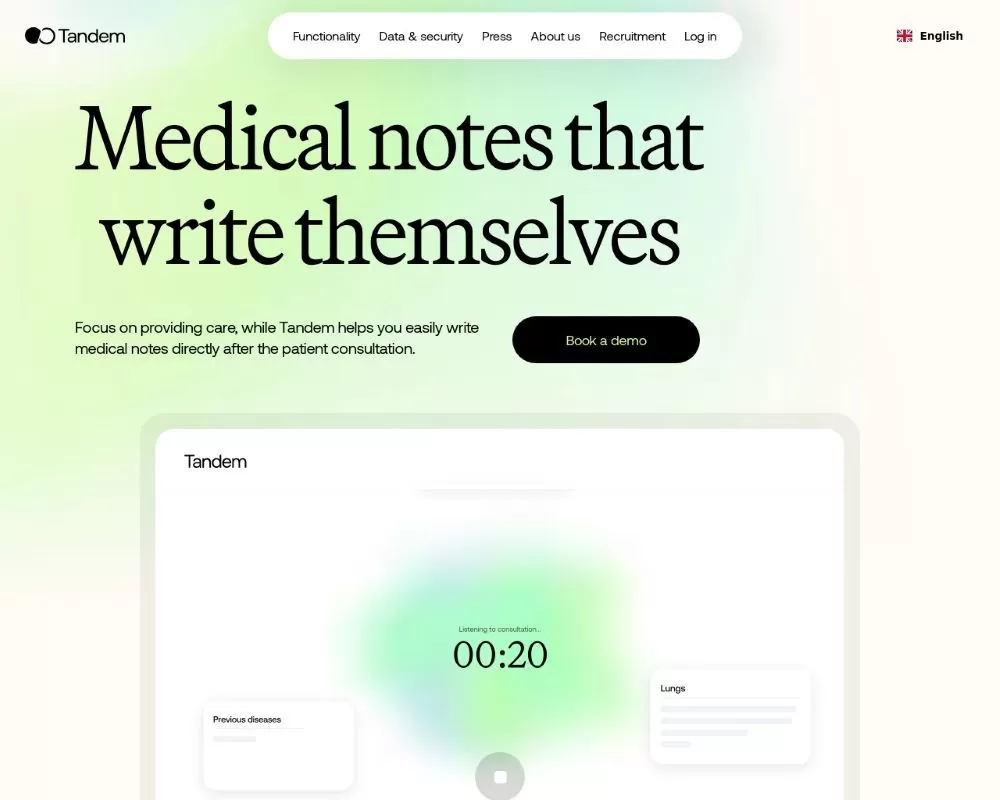
The “AI Medical Scribe | AI Clinical Notes” (Tandem ai scribe) platform is an AI-driven solution engineered to automate the documentation process in healthcare settings. By capturing doctor–patient conversations in real time, it converts spoken language into structured clinical notes (such as SOAP or customized formats) with minimal manual intervention. Built on state‐of‑the‑art speech recognition, natural language processing (NLP), and machine learning (ML) techniques, this tool promises to reduce the administrative burden on clinicians while ensuring that the quality and accuracy of patient records remain high.
Recent studies and market trends have shown that AI scribe technologies are rapidly gaining traction, with investment in the space doubling in recent years. The technology has been widely adopted by health systems and has evolved from being a mere transcription tool to a comprehensive clinical documentation assistant that helps with everything from note generation to medical coding and even predictive analysis for follow‑up care decisions.
Key Features and Functionality
Real-Time Transcription and Note Generation
-
Ambient Listening: The tool listens unobtrusively during patient encounters, capturing all the essential details without interrupting the flow of conversation.
-
Voice-to-Text Conversion: Using advanced ASR technology, the platform converts spoken language into text with high accuracy. Many users report that the real-time transcription reduces the need for post-visit note-taking.
-
Automated Summary Creation: After the encounter, the AI compiles the captured data into a well-organized note (often in SOAP format), which clinicians can review and edit.
Customization and Adaptability
-
Template Flexibility: Clinicians can choose from pre-built templates or customize their own. This flexibility is critical for different specialties—from primary care to emergency medicine and behavioral health.
-
Learning Capability: The platform can be trained to mimic individual documentation styles. Over time, it adapts to user corrections, improving accuracy and reducing editing time.
Integration with Electronic Health Records (EHR)
-
Seamless EHR Integration: The platform is designed to integrate with popular EHR systems, allowing for direct transfer of notes. This minimizes the need for copy‑and‑paste and ensures continuity of patient records.
-
Multi-Device Accessibility: Whether on a desktop, tablet, or smartphone, the tool is built to work across devices, ensuring clinicians can use it in any setting—from office visits to remote consultations.
Medical Coding and Decision Support
-
Automated Code Extraction: Beyond note-taking, the system automatically suggests ICD‑10 and CPT codes, which streamlines billing and reimbursement processes.
-
Clinical Decision Assistance: Some advanced versions incorporate features that analyze the documented information and offer clinical prompts or next‑step recommendations, further enhancing the decision‑making process.
Check this out:
Benefits and Impact of the Tandem ai scribe on Clinical Workflows
Time Savings and Efficiency
One of the most touted benefits of this AI scribe is the significant reduction in time spent on documentation. By automating note generation, clinicians save hours each week—time that can be reallocated to patient care. For example, studies and user testimonials have reported reductions of up to 50% in documentation time, translating to improved work-life balance and reduced burnout.
Enhanced Patient Interactions
By removing the distraction of manual note-taking, the platform allows clinicians to maintain better eye contact and focus more fully on their patients during consultations. This shift not only enhances the quality of the patient encounter but also boosts patient satisfaction. As one clinician noted, the ability to “listen without the keyboard” makes consultations more natural and empathetic.
Improved Accuracy and Reduced Errors
With continuous advancements in NLP and ML, the tool achieves high transcription accuracy. Although occasional errors (“hallucinations”) can occur, the overall quality of the generated notes is high enough to require only minor edits before finalizing records. This reliability is critical in ensuring that clinical documentation remains both comprehensive and precise.
Cost-Effectiveness
The subscription models for AI medical scribes vary—ranging from around $99 per month for individual providers to higher-tier enterprise plans. This predictable cost structure can offer substantial savings over hiring and training human scribes. Additionally, pay-as-you-go options are available for clinics that prefer to match costs with usage levels, making the platform accessible for practices of all sizes.
Security, Privacy, and Compliance
Given the sensitivity of medical data, the platform incorporates robust security measures:
-
HIPAA Compliance: All data transmissions are encrypted, and the platform adheres to HIPAA and other relevant data privacy regulations.
-
Data Storage and Retention: User data is handled securely, with options to process information locally or in secure cloud environments. Some platforms even offer zero‑knowledge encryption to ensure that no unauthorized party can access patient data.
-
Patient Consent Protocols: Before recording, clinicians obtain patient consent, and clear informational materials are provided to ensure transparency regarding data usage.
These measures are vital not only for regulatory compliance but also for building trust among both clinicians and patients.
Potential Drawbacks and Areas for Improvement
Occasional Transcription Errors
While the accuracy of the platform is generally high, there can be instances of misheard words or “hallucinations” where the AI generates content that was not actually spoken. Clinicians must therefore continue to review and edit the generated notes.
Dependence on Integration
The true value of the system is realized when it is fully integrated with an EHR. Without seamless integration, users may face extra steps like manual copy-and-paste, which can diminish time savings.
Learning Curve and Customization Requirements
Although the platform is designed to adapt to individual styles, initial training and customization may require additional time and effort. Some clinicians report that it takes a couple of weeks of consistent use and feedback before the system fully “learns” their preferences.
Check this out:
Comparison to Competing Solutions
The “AI Medical Scribe | AI Clinical Notes” platform competes with several similar tools such as DeepScribe, Freed, and Abridge. While each platform has its unique strengths—ranging from the speed of transcription to advanced integration and coding features—the reviewed platform stands out for its:
-
Robust Customization Options: Its ability to tailor note templates to a variety of specialties.
-
Seamless Multi-Device Support: Ensuring that clinicians have access to their documentation tool wherever they work.
-
Cost-Effective Pricing: Offering flexible subscription models that can suit both small practices and large health systems.
These factors, combined with continuous improvements in AI accuracy, make it a strong contender in a rapidly evolving market.
Future Perspectives
Looking ahead, further developments are expected to address current limitations. Enhancements may include:
-
Deeper Integration with EHR Systems: Reducing manual interventions further.
-
Improved AI Models: Utilizing more sophisticated LLMs and fine‑tuning techniques to minimize errors.
-
Expanded Clinical Decision Support: Providing real-time recommendations based on aggregated clinical data.
-
Enhanced Multilingual Capabilities: Catering to a more diverse patient population and ensuring accurate transcriptions across various accents and dialects.
As AI continues to mature, these improvements will likely increase the tool’s value proposition, helping it become an indispensable part of clinical practice.
Conclusion
The “AI Medical Scribe | AI Clinical Notes” platform represents a significant leap forward in medical documentation technology. By automating the transcription and summarization of patient encounters, it saves time, reduces administrative burdens, and enhances the quality of patient care. While there remain challenges—such as occasional transcription errors and the need for thorough EHR integration—the benefits in terms of efficiency, cost savings, and improved patient interaction are substantial.
For healthcare professionals seeking to reclaim valuable time and reduce burnout, this ambient AI scribe offers a promising solution that is both innovative and adaptable to the dynamic needs of modern medicine.
This review is based on various industry reports, academic studies, and firsthand user experiences documented in recent literature and media.